
Hypertension - B. Pharma 2nd Semester Pathophysiology notes pdf
Hypertension
Contents
Hypertension
• Definition
• Classification
• Pathogenesis
• Complications
Objective
At the end of this PDF, student will be able to
• Define hypertension
• Classify various types of hypertension
• Explain the pathogenesis involved in the development of hypertension
• Describe the complications associated with the development of hypertension
Hypertension
Persistently elevated arterial blood pressure [BP]
Associated with both functional and morphologic alteration of blood vessels
• Arterial BP - generated by the interplay between blood flow and the resistance to blood flow
• Measured in mmHg
2 types of arterial blood pressure
• Systolic BP (SBP)- achieved during cardiac contraction
• Diastolic BP (DBP)- achieved after contraction when the cardiac chambers are filling
SBP – DBP = pulse pressure (measure of arterial wall tension)
― Cardiac output - major determinant of SBP
― Total peripheral resistance determines DBP
• Mean arterial pressure [MAP] - Average pressure throughout the cardiac cycle of contraction
• During cardiac cycle 2/3rd time spent in diastole and 1/3rd time in systole
MAP= [SBP (1/3)] +[DBP (2/3)]
BP= Cardiac output × Total peripheral resistance
Clinical classification of hypertension
| Category | Systolic (mm Hg) | Diastolic (mm Hg) |
| Normal | < 130 | <85 |
| High normal | 130-139 | 85-89 |
| Hypertension | ||
| • Mild (Stage 1) | 140-159 | 90-99 |
| • Moderate (Stage 2) | 160-179 | 100-109 |
| • Severe (Stage 3) | 180-209 | 110-119 |
| • Very severe (Stage 4) | ≥ 210 | ≥ 120 |
| Malignant hypertension | > 200 | ≥ 140 |
Etiological classification of hypertension
A. Primary essential hypertension
• Genetic factors
• Racial and environmental factors
• Risk factors modifying the course of HT
B. Secondary hypertension
• Renal – Renovascular
Renal parenchymal disease
• Endocrine - Adrenocortical hyperfunction
Hyperparathyroidism
Oral contraceptives
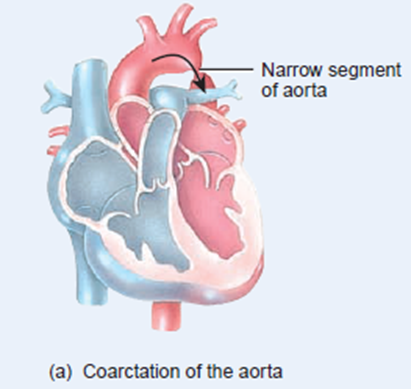
• Coarctation of aorta
• Neurogenic
Clinical classification of primary and secondary hypertension
Benign hypertension
• Observed in 95% of patients
• Slow rise in BP taking years to develop
Malignant/ accelerated hypertension
• Observed in 5-10% of patients
• Rapid rise in BP to 200/140 mm Hg or more
• If left untreated, patient’s life expectancy decreases
Symptoms of
When BP is severe, following symptoms are observed
• Nose bleeding
• Irregular heart beat
• Head ache
• Dizziness
• Fatigue
• Flushed face
• Breathing difficulties
• Strong tendency to uinate
• Vertigo, tinnitus, etc.,
Malignant hypertension is characterized by
• Pulsating headache beneath the eye
• Visual disturbance
• Nausea and vomiting
• Disturbed sleep
Pathogenesis of
BP is the product of
• Cardiac output
• Total peripheral vascular resistance
- Cardiac output
- Volume of blood that circulates through systemic blood vessels each minute
- Dependent on stroke volume (SV)
- SV - Volume of blood ejected by the left ventricle during each contraction
- Peripheral resistance depends on
̶ Viscosity of blood
̶ Diameter of the blood vessel
̶ Compliance
• High viscosity - high pressure to pass through vascular bed
• High pressure to pass through constricted and non-complaint blood vessels
BP is controlled by
- Neural component
- Peripheral auto regulatory mechanism
- Humoral mechanism
- Vascular endothelial mechanism
Neural component
• Both CNS & ANS controls BP
Centers in CNS are
̶ Vasomotor center in Medulla
̶ Vagal nucleus
̶ Area postrema
̶ Nuclues tractus solitarii
̶ Maintenance of BP by sympathetic nervous system through α and β adrenergic receptors
++ post synaptic α1 receptors ― vasoconstriction ― ↑ BP
++ pre synaptic α2 receptors ― negative feedback on NA release
++ β1 in heart ― ↑ HR and contractility
++ β2 in arterioles and venules ― vasodilation
Change in BP senses by barro receptors in carotid artery and aortic arch
• Respond to change in arterial pressure
• Transmitted to brain through IX cranial nerve and vagus nerve
• ↑ discharge from barroreceptors − depression of vasomotor center − excitation of nucleus ambiguus − reverts change in BP
Peripheral auto regulatory mechanism
• Normal case – volume and pressure adaptive mechanism of kidney maintains BP
↓ BP – adaptation of kidney ̶ more Na+ and H2O retention
↑BP – adaptation of kidney ̶ Na+and H2O excretion – ↓ blood volume & cardiac output
Humoral mechanism
- Renin Angiotensin Aldosterone system
- Natriuretic hormone
- Insulin resistance and hyperinsulinemia
Renin-Angiotensin-aldosterone system
Natriuretic hormone
• Inhibits Na+ /K+ ATP ase
• Interferes with Na+ transport across cell membrane
• ↑ Na+ in body fluids - ↑ Natriuretic hormone - ↑ urinary excretion of Na+and H2O
• Blocks active transport of Na+ out of the walls of arterioles - ↑ vascular tone and BP
Insulin resistance and hyper insulinemia
• Causes Na+ retention
• Increases sympathetic activity
• Increases vascular resistance
• Increases BP
Vascular endothelial mechanism
• Regulates blood vessel tone
• Vasodilating substances – Nitric oxide, Prostacyclin (PI2) and bradykinin – Hypotension
• Vasoconstrictors – Angiotensin II and Endothelin I - ↑BP
Effect of dietary Na+ Ca2+ K+ on BP
• ↑ intra cellular Ca2+ - alters smooth muscle function on blood vessels - ↑ Peripheral vascular resistance
• K+ depletion - ↑ Peripheral vascular resistance
• ↑ Na+ in body fluids & in arterial wall - ↑ BP
Complications of
• Blood vessels - Large arterioles dialatess
- Smaller arterioles get damaged
• Eye – Arterial narrowing, haemmorhage
• Heart - Hypertropy of left ventricles, heart failure
• Kidney – Nephrosclerosis, renal damage, death in uremia
• Brain – Rupture of damaged blood vessels, encephalopathy, cerebral edema
Summary
• Persistently elevated arterial blood pressure is called hypertension
• Hypertension can be classified as benign or malignant or accelerated hypertension
• HT can also be classifies as primary and secondary HT based on etiology
• BP is controlled by neuronal component, humoral mechanism, peripheral autoregultory mechanism and vascular endothelial mechanism
• Any defects in the functioning of these mechanisms leads to the development of HT
• HT is affects kidneys, blood vessels, brain and predisposed to many cardiovascular diseases



0 Comments: