
Disinfectant Evaluation
Disinfectant Evaluation
Contents
• Methods for disinfectant evaluation
• Bacteriostatic evaluation tests
– Serial dilution in liquid media
– Serial dilution in solid media
– Cup plate
– Ditch plate
– Gradient plate
• Evaluation of aerial disinfectants
Intended Learning objectives
At the end of this lecture, student will be able to
• Classify different methods for disinfectant evaluation
• Differentiate between bactericidal and bacteriostatic evaluation tests
• Explain the various bacteriostatic evaluation tests for disinfectants
• Explain the significance of capacity tests
• Explain the method for evaluation of solid disinfectants
Introduction
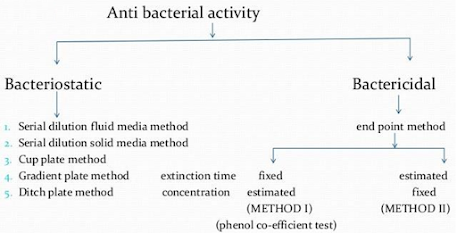
• Disinfectant evaluation – Tests used to assess bacteriostatic and bactericidal activity of disinfectants
• Bacteriostatic activity – ability of an disinfectant to stop the growth of microorganisms
• Bactericidal activity – ability to kill the organism
Tests for disinfectant activity
| SUBSTANCE TESTED | BACTERIOSTATIC TESTS | BACTERICIDAL TESTS |
| Liquid disinfectants | Serial dilution in fluid media | End-point or extinction time methods |
| | Serial dilution in solid media | Counting methods |
| | Cup-plate, fish-spine bead and filter paper methods | Turbidometric assessment |
| | Gradient-plate method | ‘In use’ and other tests |
| | Ditch-plate technique | Additional in vivo tests can be applied |
| Semi-solid antibacterial formulations, e.g. creams, ointments, pastes and gels | Cup-plate methods | Modified end-point or extinction time methods |
|
| The ditch-plate technique | Additional in vivo tests can be applied (e.g. skin tests) |
| Solid disinfectants, disinfectant powders | Inhibition on seeded agar | Modified end-point or extinction time methods |
| Aerial disinfectants | Use of slit-sampler in test chamber | |
Tests applied to liquid disinfectants Bacteriostatic activity
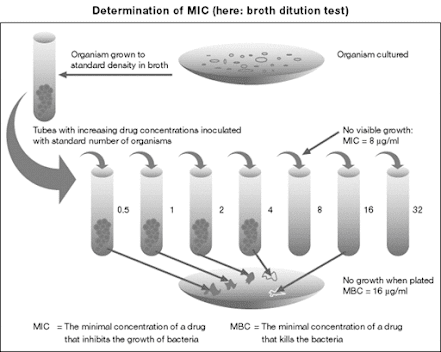
Serial dilution in fluid media
• Minimum Inhibitory Concentration (MIC) – the minimum concentration preventing detectable growth is taken as the measurement of bacteriostatic activity
• MIC varies with inoculum size, medium used and incubation conditions.
Serial dilution in solid media
1. A suitable volume of double strength nutrient agar
2. Diluted with an equal volume of bacteriostatic solution
3. Poured into sterile petri plate
4. Surface is dried by incubating at 37⁰C for 1 h
5. Drops of the test organism are placed on the dried surface
6. Incubated for 2 to 3 days
7. A separate petri dish is used for each concentration of bacteriostatic
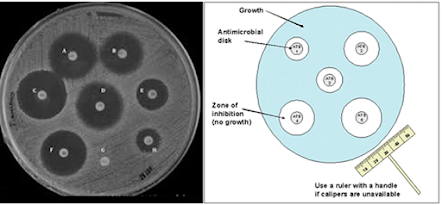
• Cup-plate, fish-spine and filter paper methods
• Agar medium is melted, cooled suitably and inoculated with the test organism
• Poured into a sterile petri dish
• Cup-plate:holes about 8 mm in diameter are cut in the agar with the help of a sterile cork borer
• Antimicrobial agent is placed in the holes
• Fish-spine bead, filter paper and cylinder method
• In all the cases, zones of inhibition may be observed
• The diameter of zones of inhibition gives rough indication of
– The relative activities of different antimicrobial substances against the test organism
– The effect of different concentrations of antimicrobial substance
The gradient - plate method
• Agar is streaked in the same line as the slope of the agar (along the concentration gradient) and reincubated.
• Approximate MIC is obtained from the equation
MIC=CX(x/y)mg/ml
C= concentration, in mg/ml, in total volume (i.e, volume of wedges A and B)
X=Length of growth, in cm
Y= total length of possible growth, in cm
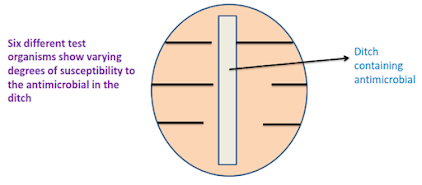
The ditch-plate technique
Carrier test
• A carrier such as a silk or catgut thread is contaminated by submersion in a liquid culture of the test organism
• The carrier is then dried and brought in contact with the disinfectant for a given exposure time
• Cultured in a nutrient broth
• No growth indicates activity of the disinfectant tested whereas growth indicates a failing.
• By multiplying the test concentrations of the disinfectant and the contact times, a potentially active concentration-time relationships of the disinfectant is obtained.
Limitations
a) The number of bacteria dried on a carrier is hard to standardize
b) The survival of the bacteria on the carrier during drying is not constant.
The AOAC Use – Dilution Test
• The AOAC Use-dilution test
• AOAC (American Association of Official Analytical Chemists)
• A carrier-based test
• Organisms: Salmonella cholerasuis, S. aureus and P. aeruginosa
• Carriers (stainless steel cylinders) are meticulously cleaned, sterilized, cooled and inoculated with a test organism by immersing in one of the culture suspensions
• The cylinders are drained on filter paper, dried at 37°C for 40 minutes, exposed to the use-dilution of the disinfectant for 10 minutes.
• After transfer from the disinfectant, the treated test surfaces are incubated in the neutralizing growth medium for 48 hours
• The number of tubes showing growth of the target microorganism is recorded.
• To “PASS" a 60 carrier test, at least 59 of the 60 surfaces tested must demonstrate complete disinfection (no detectable growth of the target microorganism in the test tubes containing neutralizing growth medium)
• To "PASS" a 10 carrier test, complete disinfection must take place on all test surfaces.
Suspension tests
• A sample of the bacterial culture is suspended into the disinfectant solution
• After exposure it is verified by subculture whether this inoculum is killed or not.
• Suspension tests are preferred to carrier tests as the bacteria are uniformly exposed to the disinfectant.
Types
A. Qualitative suspension tests:
• Loopful of bacterial suspension brought into contact with the disinfectant
• A loopful of this mixture cultured for surviving organisms.
• Results expressed as ‘growth’ or ‘no growth’.
B. Quantitative suspension tests.
• The number of surviving organisms (B) is counted and compared to the original inoculum size (A).
Microbicidal effect (ME) = Log (A) - Log (B)
• ME = 1 → killing of 90% of the initial number
• ME = 2 → 99% killed.
• A generally accepted requirement is:
• ME ≥ 5 →99.999% of the germs are killed.
Capacity test
• The ability to retain activity in the presence of an increasing load is the capacity of the disinfectant.
• In a capacity test, the disinfectant is challenged repeatedly by successive additions of bacterial suspension until its capacity to kill has been exhausted.
• Capacity tests simulate the practical situations of housekeeping and instrument disinfection.
• Best known capacity test is the Kelsey-Sykes test (Kelsey and Sykes, 1969).
Kelsy-Sykes ‘In-use’ tests
• A triple challenge test, designed to determine concentrations of disinfectant that will be effective in clean and dirty conditions.
• Organisms: 4 organisms (S. aureus, E.coli, Psedomonas aeruginosa and Proteus vulgaris)
• Three successive loads of bacteria (additions) Transfer 1ml at 0, 10, and 20 mins
• Temp: 20⁰C
• Calibrated pipette for subculture rather than loop
• Clean and dirty conditions
• Assessment (kill or not)
| Time from start (min) | Procedure |
| 0 | Inoculate 3ml of the disinfectant dilution with 1ml of bacterial suspension in broth, yeast or serum and shake gently (this gives a bactericide/bacteria reaction mixture) |
| 8 | Remove sample from above reaction mixture with a 50 dropper pipette. Transfer 1 drop to each of 5 tubes of liquid recovery media, or 5 drops to the surface of a nutrient agar plate |
| 10 | To bactericide or bacteria reaction mixture, prepared at start (time 0), add a second 1 ml of bacterial suspension |
• Sets that contain two or more negative cultures are recorded as a negative result.
• The disinfectant passes at the dilution tested if negative results are obtained after the first and second challenges.
• The third challenge is not included in the pass/fail criterion but positive cultures serve as inbuilt controls.
• If there are no positive cultures after the third challenge, a lower concentration of the disinfectant may be tested.
Tests on aerial disinfectants
• A closed room of approximately cubic dimensions and 1000cu ft capacity is used
• Fans incorporated to ensure uniform mixing of bacteria and bactericide
• Staphylococcus albus (non clumping strain) is used as the test organism
• Dispersion of organism is done using collision inhaler
• Air samples are taken using a slit sampler at suitable intervals
• The room should be initially free from extraneous microorganisms
• Temperature and humidity of air controlled
• Cyclopentanol-1-carboxylic acid is chosen as the reference standard for air disinfection
Tests applied on solid disinfectants
• Disinfectant powder is mixed with an inert substance such as talc or kieselguhr to form a disinfectant powder
• Powder is dusted onto inoculated plates
• Inert diluent is used as the control
• Alternatively Rideal Walker coefficient can also be used
• A weighed sample is shaken with distilled water at 18⁰C for 3 min
• The suspension is used for the Rideal-walker test
Summary
• Bacteriostatic tests – evaluate the property of stopping the growth of microorganisms
• Bactericidal tests – evaluate the killing property
• Bactericidal tests
– Serial dilution in solid media
– Serial dilution in liquid media
– Cup plate
– Ditch plate
– Gradient plate
• Aerial disinfectants evaluated by using a slit sampler and Staph albus as test organism
• Solid disinfectants – sprayed over the surface of a inoculated plate
For PDF Notes Click on Download Button





0 Comments: